When you click on a sponsoring school or program advertised on our site, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
This year, families will lose more than 42,000 parents, siblings, and children to breast cancer. It’s a disease health officials are trying to combat with early screenings. But getting a mammogram, often the best way to catch the cancer early, isn’t always accessible for everyone.
Medical Technology Schools analyzed data from peer-reviewed studies and the American Society of Breast Surgeons, the Centers for Disease Control and Prevention, and the American Cancer Society to illustrate the barriers that keep people from completing annual mammogram screenings for breast cancer.
The American Society of Breast Surgeons and the American Cancer Society recommend annual screenings for women over 40 at average risk for breast cancer. The risk of breast cancer is higher if an immediate relative like a parent or sibling has had it, including if that relative was a man, according to the CDC. About 500 men in the U.S. die each year from the disease.
It’s a form of cancer that affects one in eight women in their lifetime, and when caught early, the Centers for Medicare and Medicaid Services says it can be “very treatable.” Still, a majority of women—59 percent—admit to not getting screened annually, according to a 2023 poll from MedStar Health.
Cancer screenings aren’t a breeze. For breast cancer, they involve performing an X-ray of the patient’s breasts, which can reveal early signs of cancer tissue formation. The process of screening for breast cancer can be uncomfortable as it requires compressing the patient’s breast tissue for about 10-15 seconds for each image.
Fear of the screening itself, or what a patient might learn from the screening, is one reason some people choose not to get mammograms. But, studies have shown other factors can impede life-saving screenings as well.
Transportation: A Major Barrier to Access to Mammograms
Screening can help diagnose cancer early, increasing the chances a person has of surviving it—which makes the fact the majority of women in one New York study reported they faced difficulty getting mammograms all the more concerning.
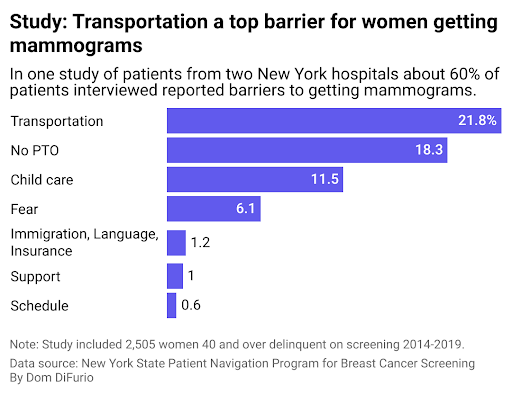
Transportation was the most common barrier to care cited by women over the age of 40 who used the New York State Patient Navigation Program for Breast Cancer Screening between 2014 and 2019. Researchers described the program as one of the most aggressive campaigns to get women screened nationwide.
Of the survey respondents who cited transportation as a barrier, only 30 percent got screened regardless of their income, suggesting transportation is a universal issue. The next most significant barrier reported was a lack of paid time off from their jobs, followed by a lack of child care. The CDC recognizes these as common barriers, along with language and the inability to visit the screening clinic frequently.
The Covid-19 pandemic presented yet another significant barrier to cancer screening appointments. Researchers estimate the health crisis delayed screening tests for as many as 9.4 million Americans in 2020. These delays have the potential to increase breast cancer deaths through 2030 by 0.5 percent, researchers suggest.
It’s a setback physicians have worked to address.
As part of the Return-to-Screening study, a joint effort by the American Cancer Society and the American College of Surgeons, 748 clinics around the country worked to increase screening for breast and other cancers from June to November 2021. Strategies implemented included raising awareness about cancer screenings and taking concerted measures to increase the number of screened, such as providing financial support and extending hours of operation.
Some clinics, like the Detroit-based Henry Ford Health, focused efforts on reducing barriers to mammograms for Black and Hispanic people, whose mammography rates were disproportionately low even before the pandemic. The organization found that fear of results and simply not realizing they needed screening were key factors preventing people from getting it. In the six-month study, improving education, among other strategies, helped increase the number of mammograms at the clinic for Black and Hispanic women by 18 and 35 percent, respectively.
Writer’s note: In this article, we have used gender-neutral terms when possible. We use gendered language in the case of direct quotations and in the characterization of data to stay true to how sources collected and presented the information.
